Research Article
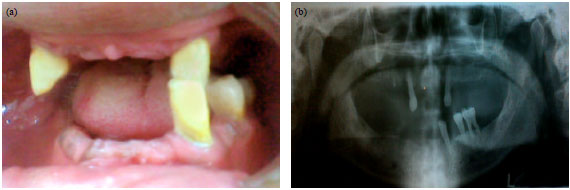
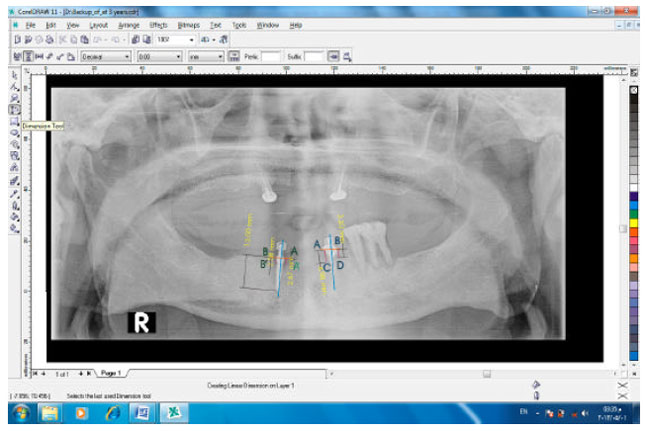
Duplicating the Implant O-ring Abutment Retainer for Using on Tooth Copy in Mandibular Implant-tooth Partial Overdenture: Radiographic Evaluations
Department of Removable Prosthodontics, Faculty of Dentistry, Mansoura University, Egypt